STEP 4: Adrenal Venous Sampling
Microadenomas cannot be reliably visualized on CT scans, and imaging does not enable radiologists to distinguish incidentalomas from aldosterone-producing adenomas.
One last step is needed in the diagnosis process — adrenal venous sampling. It is the “gold standard” test to distinguish unilateral from bilateral disease, and to determine the best course of treatment.
It is also a complex test whose success rate largely depends on the case volume handled by diagnostic centers, and on the skills and expertise of their interventional radiologists.
Purpose of AVS and How it is Performed
Adrenal venous sampling addresses whether the autonomous aldosterone production identified in step 2 of the diagnosis process is affecting one (unilateral disease) or both adrenal glands (bilateral disease).
The test consists in collecting cortisol and aldosterone samples at the closest possible source: the adrenal veins.
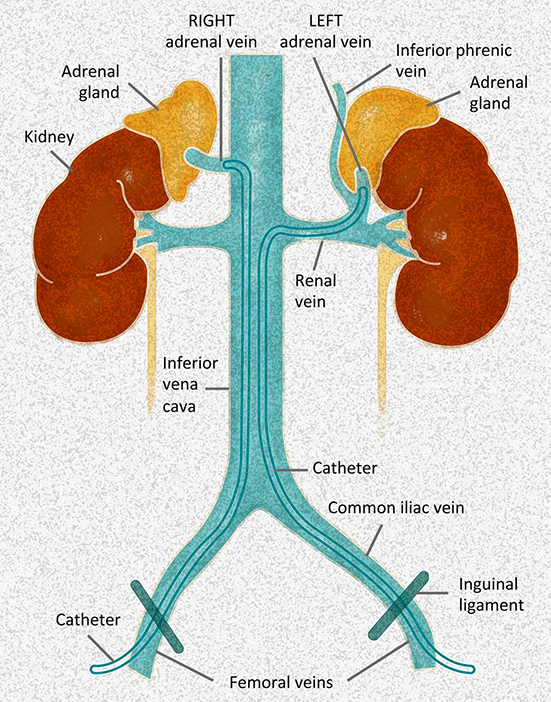
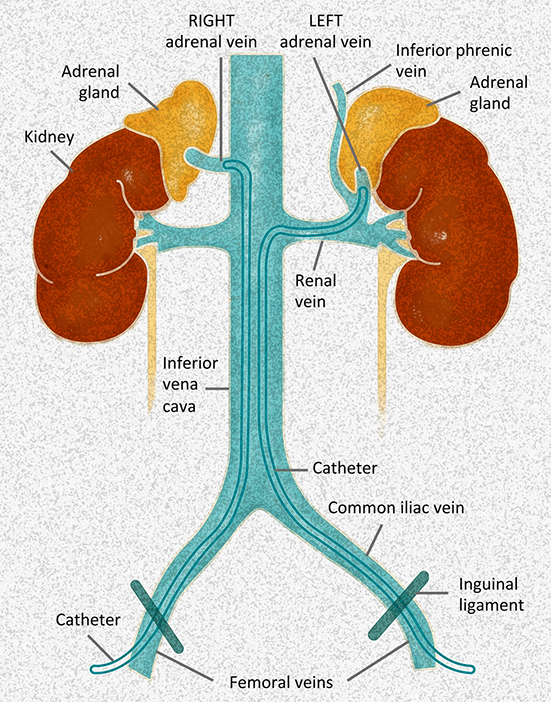
Because the right adrenal vein originates in the inferior vena cava (IVC), it is usually more difficult to canulate. The left adrenal vein directly originates in the left renal vein, and is usually less challenging to cannulate. Various catheters may be needed to accurately sample both sides.
The procedure is performed by an interventional radiologist in a hospital radiology suite with patients placed under “conscious sedation” (they remain awake, but do not feel any pain).
The radiologist starts with making a small puncture in the femoral vein (groin) or jugular vein (neck), and threads a small catheter until it reaches the right adrenal vein. The radiologist then takes a blood sample from the adrenal vein.
The same steps are repeated on the opposite side to sample the left adrenal vein, and a blood sample is also taken from the IVC or femoral vein for reference.
All blood samples are labeled in their individual tubes, and sent to a lab for analysis. Results are usually available within a week.
Source: Diagnosis and Management of Primary Aldosteronism: the Endocrine Society Guideline 2016 Revisited ©Bioscientifica. Used with permission.
Purpose of AVS and How it is Performed
Adrenal venous sampling addresses whether the autonomous aldosterone production identified in step 2 of the diagnosis process is affecting one (unilateral disease) or both adrenal glands (bilateral disease).
The test consists in collecting cortisol and aldosterone samples at the closest possible source: the adrenal veins.
Because the right adrenal vein originates in the inferior vena cava (IVC), it is usually more difficult to canulate. The left adrenal vein directly originates in the left renal vein, and is usually less challenging to cannulate. Various catheters may be needed to accurately sample both sides.
The procedure is performed by an interventional radiologist in a hospital radiology suite with patients placed under “conscious sedation” (they remain awake, but do not feel any pain).
The radiologist starts with making a small puncture in the femoral vein (groin) or jugular vein (neck), and threads a small catheter until it reaches the right adrenal vein. The radiologist then takes a blood sample from the adrenal vein.
The same steps are repeated on the opposite side to sample the left adrenal vein, and a blood sample is also taken from the IVC or femoral vein for reference.
All blood samples are labeled in their individual tubes, and sent to a lab for analysis. Results are usually available within a week.
Cosyntropin Stimulation
Adrenal glands do not produce cortisol and aldosterone in a continuous stream, and when one side is sampled after the other, the samples may not represent the actual values.
Sampling both sides at the same time is an option to remediate this risk. Unless performed by a very skilled radiologist, this method is however associated with a risk of adrenal vein thrombosis.
As a result, some diagnostic centers prefer to pharmacologically stimulate the adrenal glands with an infusion of cosyntropin (a synthetic version of ACTH) to ensure that veins are adequately sampled.
Since one has not been proven superior to the other, the choice of method is left at the discretion of the diagnostic center. It is however recommended to consistently use one method or the other, and use higher cutoff values for the selectivity index and lower cutoff values for the lateralization index with pharmacological stimulation.
Call to Action
AVS is the most effective test available to decide whether primary aldosteronism should be treated surgically or medically.
Yet the impact of cosyntropin stimulation on disease outcome remains unknown, and the accuracy of AVS remains a concern. A study published in November 2020 demonstrated that because aldosterone production is highly variable, obtaining multiple measurements may provide more reliable interpretation of AVS results than single measurements.
If you or someone you know has long-standing and/or hard to control hypertension, we invite you to sign the Foundation’s Open Letter to help us advocate optimum diagnosis and treatment of primary aldosteronism.
How to Prepare for the Test and What to Expect Afterwards
Like ARRs, AVS results are influenced by sodium intake, potassium level, and blood pressure medications. Preparation for AVS is the same as for ARR . Compliance with these recommendations has a direct impact on the accuracy of results, and should be optimized by physicians and patients alike.
The test is usually performed in a couple of hours, and since it only involves mild sedation, patients are discharged within 2 to 4 hours. When the AVS is performed via the groin, patients must lay flat for up to 4 hours after the procedure. When it is performed via the neck, patients can recover in the seated position. The AVS involves a puncture in the skin, and it is normal to feel soreness or tenderness at the sites for a short period of time. Upon returning home, patients should not stay alone, and should refrain from taking a shower, driving and operating any equipment for 24 hours.
To prevent undue stress on the procedure sites, it is recommended to rest for 72 hours, to refrain from lifting anything heavier than 10 pounds, and to use caution when climbing stairs or changing positions.
If bleeding occurs, pressure should be applied with a clean towel for 5 minutes uninterrupted. If bleeding is significant or does not stop, it is recommended to promptly call 911, and continue to hold pressure on the site until paramedics arrive.
What Results Mean
Selectivity
AVS results must first show that the adrenal veins were correctly sampled. This is why samples are taken as reference from another vein than the adrenal veins – usually the inferior vena cava. The cortisol level in each adrenal vein (CAV) is compared to the peripheral sample taken from the inferior vena cava (Cperipheral) to produce a ratio equal to CAV/Cperipheral called “Selectivity Index.” The cortisol in the adrenal veins should be several times greater than in the peripheral sample. When AVS is performed with cosyntropin stimulation (i.e., preferred method), a cutoff value of 5 and above is indicative of a successful procedure. When the AVS is performed without stimulation, a cutoff value of 2 and above is recommended.
| Lab Results | Selectivity Index (SI) |
|---|---|
Cortisol Left Adrenal: 69.2 ug/dL |
Left SI: 69.20 / 9.00 = 7.7 |
This AVS was performed without cosyntropin stimulation (with cosyntropin the cortisol concentrations are typically 400-800 μg/dL). The ratio on both sides is above 2, so the veins have been sampled properly. Had the ratio been below 2, the samples could not have been used.
Lateralization
Once sampling has been validated, a “Lateralization Index” is used to determine whether one side is responsible for the over secretion of aldosterone. The aldosterone level in each sample (left: ALAV; right: ARAV) is normalized to the cortisol level in each sample (left: CLAV; right: CRAV) to produce two ratios: ALAV/CLAV, and ARAV/CRAV. Next, the aldosterone to cortisol ratio on the dominant side (i.e. the side with the highest aldosterone to cortisol ratio) is divided by the aldosterone to cortisol ratio on the contralateral side.
When AVS is performed with stimulation (i.e., preferred method), a result greater than 4 is indicative of a unilateral source of aldosterone, and a result lower than 4 is indicative of bilateral disease. Results between 3 and 4 require interpretation in light of other diagnostic tests, and repeat AVS should be considered. When AVS is not performed with stimulation, the lateralization index must be greater than 2 to be indicative of unilateral disease.
| Lab Results | Lateralization Index (LI) |
|---|---|
Cortisol Left Adrenal Vein: 69.2 ug/dL |
ALAV/CLAV: 3651 / 69.2 = 52.8 |
CT imaging showed an adenoma on the left adrenal gland of this patient. The lateralization index is above 4. The left adenoma is the cause of aldosterone oversecretion.
| Lab Results | Lateralization Index (LI) |
|---|---|
Cortisol Left Adrenal Vein: 12.5 mcg/dL |
ALAV/CLAV: 52.9 / 12.5 = 4.2 |
An adenoma had been previously seen during CT imaging on the right adrenal gland of this patient. The lateralization index is below 4. The adenoma is not causing excess aldosterone. The patient has bilateral disease.
Contralateral Suppression
Most diagnostic centers use the Lateralization Index alone to diagnose unilateral disease. Evidence shows that contralateral gland suppression can also help to determine lateralization. This method consists in comparing ratios: when the aldosterone-cortisol ratio in the contralateral adrenal vein is no higher than in the peripheral vein, unilateral disease is considered to be likely.
AVS Calculator
The Foundation’s calculator was designed to help you understand your AVS results. It uses the cutoff values recommended by the Endocrine Society Guidelines. It is built for the sole purpose of helping you visualize how AVS results are computed. It is not a substitute for medical interpretation. Only your physicians can provide advice and recommendations about your health based on your results. Mathematical operations are run directly on your local computer. None of your data can be accessed over the Internet or collected by the Primary Aldosteronism Foundation, either when you enter it or when the calculator returns results.
How to Use the Calculator
- Enter the cortisol values for your right and left adrenal glands, and inferior vena cava or femoral vein
- Enter the aldosterone values in the same way
- Select whether cosyntropin stimulation was used during your procedure
- Press the “Submit” button, and the values for your AVS together with their standard interpretation will display. If the adrenal veins were not sampled correctly, the calculator will indicate that results are inconclusive.
Note
On your lab report, aldosterone and cortisol results may be listed in the middle of other tests. Cortisol measurements may be listed as μg/dL, mcg/dL, or nmol/L. Aldosterone measurements will be listed as either ng/dL or pmol/L.
Hyperaldosteronism and Subclinical Cushing’s Syndrome
Also called concomitant mild autonomous cortisol secretion (MACS), subclinical Cushing’s syndrome (SCS) occurs when an adrenal adenoma secretes cortisol in a way that is ACTH-independent and not fully restrained by pituitary feedback. SCS causes hypertension, insulin resistance and dyslipidemia, and coexists with hyperaldosteronism 10 to 20% of the time.
Patients with a known adrenal adenoma should therefore be evaluated for SCS. To do so, an overnight dexamethasone test is performed with a single dose of 1 mg of dexamethasone taken between 11:00 PM and midnight. Serum cortisol is drawn between 8 and 9:00 AM the next day. Levels of 1.8 mcg/dL (50 nmol/L) and above are considered positive for SCS with a diagnostic sensitivity of 95%.
When both diseases coexist, it is essential to determine whether hormonal overproduction is caused by unilateral disease and could be remediated by surgery. Multiple case scenarios are possible that include, among others, adenoma co-secreting aldosterone and cortisol, aldosterone and cortisol overproduction originating in different adrenal glands, aldosterone-producing adenoma with bilateral overproduction of cortisol. AVS alone may be able to identify these possible cases. However, confirming successful catheterization and lateralization is challenging with SCS because of uneven cortisol co-secretion.
Young et al. recommend measuring plasma epinephrine to determine successful cannulation of the adrenal veins: epinephrine concentration in the AV must be 100 pg/ml above the IVC (AV–IVC >100 pg/ml). Young et al. also recommend using cortisol lateralization ratios: AV/PV cortisol ratio should be above 6.5 on one side and below or equal to 3.3 on the contralateral side. A cortisol lateralization ratio above or equal to 2.3 indicates unilateral cortisol-secretion while a ratio below or equal to 2 indicates bilateral cortisol hypersecretion.
SCS significantly increases AVS and treatment complexity (e.g., adrenal insufficiency post-adrenalectomy, need for bilateral adrenalectomy). Patients with primary aldosteronism and SCS should therefore seek care at centers of excellence with experience in treating this more complex form of hyperaldosteronism.
Risks Associated with AVS

Adrenal venous sampling is an invasive test that involves a complex technique that only skilled and experienced interventional radiologists can perform with a satisfactory success rate of 90% or more.
Other than Centers of Excellence, very few diagnostic centers achieve such a rate consistently for their patient population.
This poses a significant risk to patients:
- Erroneous results lead to erroneous diagnosis;
- More often, AVS results are found to be inconclusive. Patients have to undergo the procedure multiple times, or seek care at a different center far from home to repeat the test.
The correct location of the catheters is confirmed with injection of a contrast agent. Radiation exposure is thus inherent to adrenal venous sampling. Notable differences exist among diagnostic centers, and patients should enquire whether their center applies standard operating procedures to limit radiation exposure.
At Centers of Excellence, the complication rate is believed to be 2.5% or less. The most common complications include symptomatic groin hematoma, adrenal hemorrhage, and dissection of an adrenal vein. Nerve damage, infarction, adrenal vein thrombosis, hypertensive crisis, and adrenal insufficiency have been reported.
Rupture of an adrenal vein and subsequent hemorrhage are considered a major complication. It may cause extensive retroperitoneal adhesions which, in turn, may make laparoscopic adrenalectomy more difficult. Its rate is less than 1% at centers with a dedicated AVS program.
Patients should not undergo AVS unless they have the certainty that their diagnostic center handles a high enough case volume, and employs skilled radiologists who have a robust track record of successful AVS procedures.
References
- Funder, J. W., Carey, R. M., Mantero, F., Murad, M. H., Reincke, M., Shibata, H., Stowasser, M., & Young Jr, W. F. (2016). The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 101(5), 1889-1916.
- Williams, T. A., & Reincke, M. (2018). Management of endocrine disease: diagnosis and management of primary aldosteronism: the Endocrine Society guideline 2016 revisited, European Journal of Endocrinology, 179(1), R19-R29.
- Wolley, M. J., Gordon, R. D., Ahmed, A. H., & Stowasser, M. (2015). Does contralateral suppression at adrenal venous sampling predict outcome following unilateral adrenalectomy for primary aldosteronism? A retrospective study. The Journal of Clinical Endocrinology Metabolism, 100(4), 1477-1484.
- Laurent, I., Astère, M., Zheng, F., Chen, X., Yang, J., Cheng, Q., & Li, Q. (2019). Adrenal venous sampling with or without adrenocorticotropic hormone stimulation: a meta-analysis. The Journal of Clinical Endocrinology Metabolism, 104(4), 1060-1068.
- Rossi, G. P., Barisa, M., Allolio, B., Auchus, R. J., Amar, L., Cohen, D., Degenhart, C., Deinum, J., Fischer, E., Gordon, R., Kickuth, R., Kline, G., Lacroix, A., Magill, S., Miotto, D., Naruse, M., Nishikawa, T., Omura, M., Pimenta, E., Plouin, P-F., Quinkler, M., Reincke, M., Rossi, M., Rump, L. C., Satoh, F., Kool, L. S., Seccia, T. M., Stowasser, M., Tanabe, A., Trerotola, S., Vonend, O., Widimsky, J., Wu, K-D, Wu, V-C., & Pessina, A. C. (2012). The adrenal vein sampling international study (AVIS) for identifying the major subtypes of primary aldosteronism. The Journal of Clinical Endocrinology Metabolism, 97(5), 1606-1614.
- Yozamp, N., Hundemer, G. L., Moussa, M., Underhill, J., Fudim, T., Sacks, B., & Vaidya, A. (2021). Variability of aldosterone measurements during adrenal venous sampling for primary aldosteronism. American Journal of Hypertension, 34(1), 34-45.
- Rossitto, G., Amar, L., Azizi, M., Riester, A., Reincke, M., Degenhart, C., Widimsky Jr, J., Naruse, M., Deinum, J., Schultzekool, L., Kocjan, T., Negro, A., Rossi, E., Kline, G., Tanabe, A., Satoh, F., Rump, L. C., Vonend, O., Willenberg, H. S., Fuller, P., Yang, J., Yong, N., Chee, N., Magill, S. B., Shafigullina, Z., Quinkler, M., Oliveras, A., Chang, C-C., Wu, V-C., Somloova, Z., Maiolino, G., Barbiero, G., Battistel, M., Lenzini, L., Quaia, E., Pessina, A. C., & Rossi, G. P. (2020). Subtyping of primary aldosteronism in the AVIS-2 study: assessment of selectivity and lateralization. The Journal of Clinical Endocrinology Metabolism, 105(6), 2042-2052.
- Hu, L., Ji, W., Guo, M., Yi, T., Wang, J., Bao, M., Gao, Y., Jin, H., Lu, D., Ma, W., Han, X., Li, J., & Yuan, Z. (2022). Case report: primary aldosteronism and subclinical Cushing syndrome in a 49-year-old woman with hypertension plus hypokalaemia. Frontiers in Cardiovascular Medicine, 9, 911333.
- Dogra, P., & Vijayashankar, N. P. (2023). Dexamethasone Suppression Test. In StatPearls [Internet]. Treasure Island. https://www.ncbi.nlm.nih.gov/books/NBK542317/
- Young Jr, W. F., du Plessis, H., Thompson, G. B., Grant, C. S., Farley, D. R., Richards, M. L., Erickson, D., Vella, A., Stanson, A. W., Carney, J. A., Abboud, C. F., & Carpenter, P. C. (2008). The clinical conundrum of corticotropin-independent autonomous cortisol secretion in patients with bilateral adrenal masses. World Journal of Surgery, 32(5), 856-62.

