PA is Under-Diagnosed
Primary Aldosteronism is Missed or Misdiagnosed 95% of the Time
In a retrospective cohort study of 4,660 patients with resistant hypertension in California, the screening rate for primary aldosteronism was 2.1%.
An Australian study found that in a group of 87 hypertensives, 69.2% had indications for primary aldosteronism, but only 3.2% were actually screened. At the time of referral to the country’s national health service, 61% of the patients had had hypertension for over 10 years, and 42% of the patients had developed end-organ damage.
Primary Aldosteronism is Not Rare
In 2020, The Unrecognized Prevalence of Primary Aldosteronism unequivocally showed that PA is a highly prevalent syndrome that represents a major public health issue. Based on this study and on 2021 US census data: 40 million Americans aged 18 or older have PA. This equals to 1 in 8 Americans, or 12% of the US population.
Even with a prevalence 3 times lower than this, PA would affect:
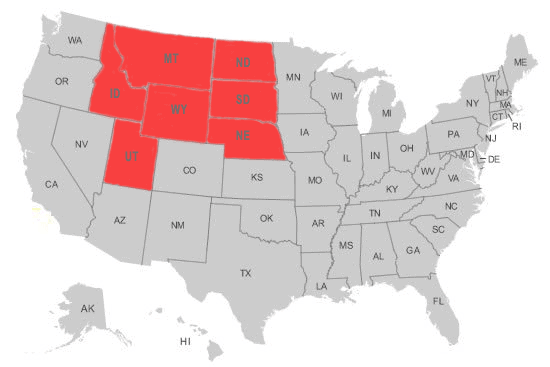
- In the US: the equivalent of the entire population of the states of Wyoming, Montana, Idaho, North and South Dakota, Nebraska, and Utah combined, or
- Worldwide: the equivalent of the entire population of the UK, France, Italy, and Spain combined.
US Population Equivalent
under 4% Prevalence
Worldwide Population Equivalent
under 4% Prevalence

Why Primary Aldosteronism is Under-Diagnosed
Primary aldosteronism is mistakenly considered rare. The definition of “rare disease” varies across countries. In the US, a disease is considered rare when it affects less than 200,000 people. In Europe, a condition is defined as rare when fewer than 2,000 individuals are affected. In all evidence, hyperaldosteronism does not meet the criteria of these definitions. The disease is “believed” to be rare while, in fact, it is widespread.
Inadequate physician training. The common misbelief that primary aldosteronism is rare is embedded in medical education. It particularly affects primary care and internal medicine physicians who are not cautioned that hyperaldosteronism is widespread, and must be promptly and adequately diagnosed.
Lack of research. Understanding of excess aldosterone remains fragmented, and its measurement threshold (12.0 g per 24 hours) arbitrary. While a cut-off value is needed to enable case detection, this value is currently so high that even systematic screening would miss a significant number of patients.
Lack of standardization. Fragmented understanding of the disease equally affects diagnostic protocols. Among others:
- While Aldosterone Renin Ratios are widely available, assays vary across laboratories, thereby rendering their accuracy and reliability questionable.
- The modalities of confirmatory testing range from the ingestion of salt tablets at home to a saline infusion done under medical supervision.
- Some medical centers use ACTH stimulation to determine the disease subtype, while others do not.
Testing cost and complexity. Workup is not complete without adrenal venous sampling, a procedure few medical centers can successfully offer to their patients since it can only be performed by experienced interventional radiologists. Not only is the procedure costly, its low success rate outside of expert centers leads to repeat testing, and in extreme cases, erroneous surgical recommendations.
References
- Brown, J. M., Siddiqui, M., Calhoun, D. A., Carey, R. M., Hopkins, P. N., Williams, G. H., & Vaidya, A. (2020). The unrecognized prevalence of primary aldosteronism: a cross-sectional study. Annals of Internal Medicine, 173(1), 10-20.
- Funder, J. W. (2020). Primary aldosteronism: at the tipping point. Annals of Internal Medicine, 173(1), 65-66.
- Reincke, M., Beuschlein, F., & Williams, T. A. (2020). Progress in primary aldosteronism 2019: new players on the block? Hormone and Metabolic Research, 52(6), 345-346.
- Monticone, S., Burrello, J., Tizzani, D., Bertello, C., Viola, A., Buffolo, F., Gabetti, L., Mengozzi, G., Williams, T. A., Rabbia, F., Veglio, F., & Mulatero, P., Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. Journal of the American College of Cardiology, 69(14), 1811-1820.
- Lim, Y. Y., Shen, J., Fuller, P. J., & Yang, J. (2018). Current pattern of primary aldosteronism diagnosis: delayed and complicated. Australian Journal of General Practice, 47(10), 712-718.
- Hannemann, A., & Wallaschofski, H. (2012). Prevalence of primary aldosteronism in patient’s cohorts and in population-based studies – A review of the current literature. Hormone and Metabolic Research, 44(3),157-62.
- Rossi, E., Perazzoli, F., Negro, A., & Magnani, A. (2017). Diagnostic rate of primary aldosteronism in Emilia‐Romagna, Northern Italy, during 16 years (2000–2015). Journal of Hypertension, 35(8), 1691-1697.

