Blood Pressure Monitoring
Patients who have primary aldosteronism must closely monitor their blood pressure. Since their hypertension can be difficult to control, and their blood pressure can be labile (i.e., readings can vary a lot and abruptly), the accuracy and reliability of measures taken by patients and healthcare professionals are very important:
- Falsely low readings mean treatment will not sufficiently lower blood pressure, and
- Falsely high readings mean patients will be overmedicated.
What is Measured?
Blood pressure is measured in millimeters of mercury (mmHg), and involves two figures:
- Systolic pressure: pressure from the blood on the artery when the heart beats, and
- Diastolic pressure: pressure from the blood on the artery when the heart rests between beats.
For example, a blood pressure reading of 152/93 means a systolic pressure of 152 mmHg, and a diastolic pressure of 93 mmHg. Although the systolic pressure tends to receive more attention, either measure is used to diagnose hypertension.
What the Measures Mean
Blood pressure categories range from normal to elevated, hypertension stage 1, hypertension stage 2, and hypertensive crisis.
To be considered within normal range, blood pressure must be less than 120/80.
Untreated, hyperaldosteronism can cause dangerously high blood pressure. Patients should thus be vigilant to ensure optimal control of their hypertension.
| Blood Pressure | Systolic | Diastolic | |
|---|---|---|---|
| Normal | Less than 120 | and | Less than 80 |
| Elevated | 120 - 129 | and | Less than 80 |
| Hypertension - Stage 1 | 130 -139 | or | 80-90 |
| Hypertension - Stage 2 | 140 or higher | or | 90 or higher |
| Hypertension Crisis | Higher than 180 | and/or | Higher than 120 |
White Coat Syndrome and Masked Hypertension
Patients whose blood pressure is higher when taken in a medical setting than at home have what is called “white coat syndrome.” The reverse situation, i.e. when blood pressure is higher at home than at a physician’s office, is called “masked hypertension.” Awareness of the condition is important since it leads to inaccurate measures, and possibly misdiagnosis.
To prevent these errors, blood pressure is not solely assessed with in-office measures. Instead, patients are requested to wear a device that measures blood pressure over a longer period of time (usually 24 hours) outside the medical setting. This method is called ambulatory blood pressure monitoring.
Because they are more vulnerable to stress and anxiety, patients who have primary aldosteronism may have higher blood pressure readings in a medical setting.
Hypertensive Crises
Hypertensive crises are defined as a blood pressure higher than 180/120. As long as they remain undiagnosed or encounter difficulties with treatment, patients with primary aldosteronism are susceptible to hypertensive crises.
The consequences of such elevated levels can be severe and include stroke, heart attack, damage to the eyes and kidneys, loss of kidney function, and aortic dissection.
A blood pressure reading of 180/120 and above should be followed by an additional reading within five minutes. If there is no improvement, since hypertensive crises are considered a medical emergency, calling 911 or going to the nearest emergency room is indicated at that point (even more so when readings are accompanied by symptoms such as chest pain, shortness of breath, numbness/weakness or change in vision).
Blood Pressure vs. Pulse
The pulse, or heart rate, is the number of times the heart beats in a minute. At rest, when the heart pumps the lowest amount of blood (when we are sitting or lying), a normal pulse is between 60 and 100 beats per minute. Low to moderate physical activity doesn’t trigger significant change in heart rate but exercise does, and the change increases with the intensity of the exercise.
Patients with primary aldosteronism can experience faster heart rate, even at rest. When they exercise, their pulse can also be much higher than healthy individuals, and it may take longer for their heart rate to get back to baseline after they exercise.
How is it Measured?
Be it at a physician’s office or at home, blood pressure should be measured in a quiet setting. The recommended position is sitting in a straight chair with back support, arms resting on a table, feet resting flat on the floor, and legs uncrossed:
- The absence of back and feet support falsely increases blood pressure,
- Laying down falsely lowers blood pressure.
Blood pressure is slightly different in both arms. One side is usually higher than the other, and should be the side used for ongoing monitoring. Because of this difference, it is important to make sure that arm support can be provided on both sides. Using the proper size cuff is also essential. The cuff should be placed directly above the antecubital fossa, and its center should be placed at heart level:
- If the cuff is placed too high or is oversized, measures will be falsely low,
- If the cuff is placed too low or is undersized, measures will be falsely elevated.
Blood pressure should be measured three times consecutively with at least a one-minute interval between measures. The first reading should be discarded, and the last two should be averaged to produce the final measure. At home, blood pressure should be monitored at the same time every day, preferably once in the morning and once in the evening. To avoid discrepancies, measures should be compiled instead of relying on subjective recollection.
Methods and Devices

Mercury sphygmomanometer
(ADC Diagnostix 952)

Aneroid sphygmomanometer
(ADC Prosphyg 775)
Auscultatory method. In clinical settings, blood pressure is often measured using a stethoscope and a sphygmomanometer (a manually inflatable cuff connected to a mercury or aneroid manometer).
The stethoscope is used to listen to the brachial artery for sounds made by blood flow under the cuff. When the cuff is inflated, the pressure applied to the arm prevents blood from flowing, and no sound can be heard. With deflation, blood is allowed to flow again, and successive sounds are heard. The initial sound corresponds to the systolic pressure, and the final sound to the diastolic pressure.
Because the auscultatory method can be affected by environmental noise, the practitioner’s hearing or even observer bias, the use of automated devices is becoming more widespread in clinical settings.
Methods and Devices
Auscultatory method. In clinical settings, blood pressure is often measured using a stethoscope and a sphygmomanometer (a manually inflatable cuff connected to a mercury or aneroid manometer).
The stethoscope is used to listen to the brachial artery for sounds made by blood flow under the cuff. When the cuff is inflated, the pressure applied to the arm prevents blood from flowing, and no sound can be heard. With deflation, blood is allowed to flow again, and successive sounds are heard. The initial sound corresponds to the systolic pressure, and the final sound to the diastolic pressure.
Because the auscultatory method can be affected by environmental noise, the practitioner’s hearing or even observer bias, the use of automated devices is becoming more widespread in clinical settings.

Mercury sphygmomanometer
(ADC Diagnostix 952)

Aneroid sphygmomanometer
(ADC Prosphyg 775)
Methods and Devices
In clinical settings, blood pressure is often measured using the auscultatory method, i.e. with a stethoscope and a sphygmomanometer (a manually inflatable cuff connected to a mercury or aneroid manometer). The stethoscope is used to listen to the brachial artery for sounds made by blood flow under the cuff. When the cuff is inflated, the pressure applied to the arm prevents blood from flowing, and no sound can be heard. With deflation, blood is allowed to flow again, and successive sounds are heard. The initial sound corresponds to the systolic pressure, and the final sound to the diastolic pressure. Because the auscultatory method can be affected by environmental noise, the practitioner’s hearing or even observer bias, the use of automated devices is becoming more widespread in clinical settings.
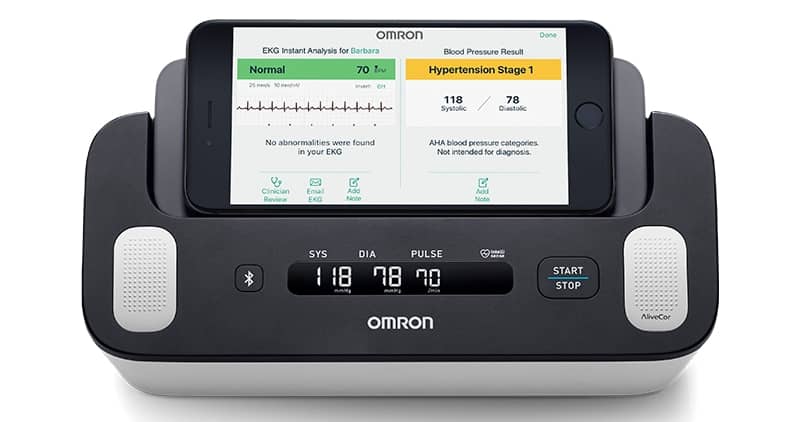
(Omron BP7900)

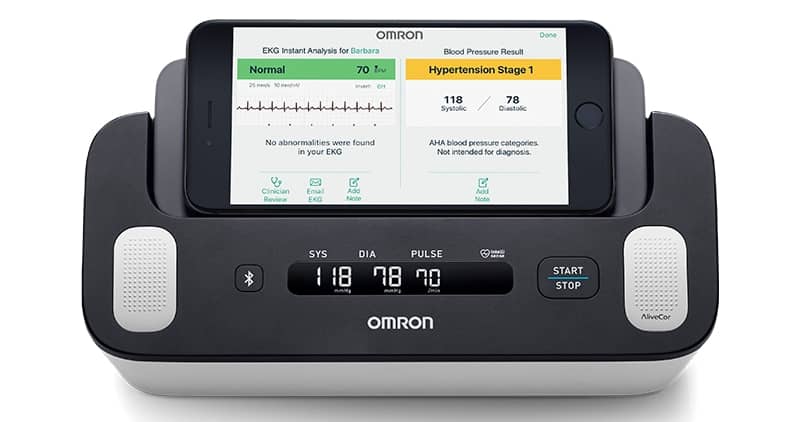
Oscillometric method. Home monitoring devices use a method based on vibrations caused by blood flow in the arterial wall. The cuff of these devices inflates and deflates automatically, electronic sensors record cuff pressure oscillations, and an algorithm interprets these oscillations to determine the systolic and diastolic pressure. Selecting the correct cuff size is important when purchasing a home monitoring device. The American Heart Association recommends cuff-style, upper-arm home monitors instead of smart apps, wrist and finger devices as they yield less reliable readings or have not been rigorously tested. Since the cuff fit affects the accuracy of readings, patients should measure their arm circumference and choose the correct size cuff:
- Adult small: arm circumference of 22 to 26 cm (8.5 to 10 in),
- Adult average: arm circumference of 27 to 34 cm (10.5 to 13 in),
- Adult large: arm circumference of 35 to 44 cm (13.5 to 17 in).
Measurements taken with home devices vary based on the algorithms used by manufacturers. The ability of these devices to produce accurate measurement is essential to manage hypertension. The American Medical Association has established criteria to validate the clinical accuracy of automated devices available in the US. The list of devices can be found on Validate BP, a website dedicated to the initiative. To ensure that readings are accurate, patients should also ask their physician to validate their device by obtaining simultaneous readings with their home device and the auscultatory method.
Some devices are available with Bluetooth or Wi-Fi wireless connections to upload measurements to smartphones and computers for recordkeeping or sharing with your physician.
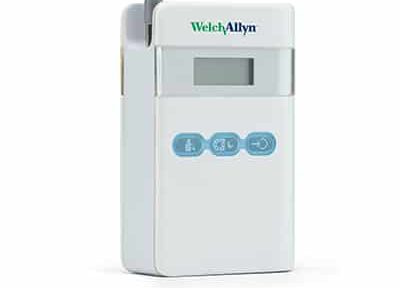
Ambulatory blood pressure monitoring is an automated method used to record measures at regular intervals over a 24-hour period when white-coat syndrome is suspected or more representative measures are needed.
Blood pressure usually rises in the daytime and falls after midnight. The early morning fall is called “night-time dip” and can be detected by ambulatory blood pressure monitoring.
This is particularly relevant for patients affected by primary aldosteronism since non-dipping blood pressure is associated with a higher risk of left ventricle hypertrophy and cardiovascular mortality. The device can also be used to monitor treatment effectiveness and ensure that blood pressure is well controlled throughout the day and night.
References
- Shimbo, D., Artinian, N. T., Basile, J. N., Krakoff, L. R., Margolis, K. L., Rakotz, M. K., Wozniak, G., & American Heart Association and the American Medical Association. (2020). Self-measured blood pressure monitoring at home: a joint policy statement from the American Heart Association and American Medical Association. Circulation, 142(4), e42-e63.
- American Heart Association (2020). High Blood Pressure. https://www.heart.org/en/health-topics/high-blood-pressure.
- Grim, C. E., & Grim, C. M. (2001). Accurate and reliable blood pressure measurement in the clinic and home: the key to hypertension control. In Hollenberg, N. K. (Eds.), Atlas of Heart Diseases: Hypertension Mechanisms and Therapy (pp. 314-324). Current Medicine Group.
- Grim, C. E., & Grim, C. M. (2016). Auscultatory BP: still the gold standard. Journal of the American Society of Hypertension, 10(3), 191-193.
- Eguchi, K., Kuruvilla, S., Ogedegbe, G., Gerin, W., Schwartz, J. E., & Pickering, T. G. (2009). What is the optimal interval between successive home blood pressure readings using an automated oscillometric device? Journal of Hypertension, 27(6), 1172-1177.
- Lewis, P. S., & British and Irish Hypertension Society. (2019). Oscillometric measurement of blood pressure: a simplified explanation. A technical note on behalf of the British and Irish Hypertension Society. Journal of Human Hypertension, 33(5), 349-51.



